Medical misdiagnosis survey sheds light on worrying misdiagnosis trends and continuously overlooked symptoms in women’s health.
Diagnosis can be a matter of life and death, and while all individuals are at risk of medical misdiagnosis, evidence indicates that the issue disproportionately impacts women. Whether this is a consequence of sex and gender medicine being generally understudied [1], medical gaslighting (both intentional and unconscious) [2], society’s social issues [3], or perceived female “hysteria” [4].
To better understand and highlight misdiagnosis as a gendered issue, Higgs LLP surveyed 500 women who have experienced an incorrect diagnosis. The survey aimed to raise awareness about the wrongly diagnosed symptoms, associated timescales, and incorrectly prescribed medication, highlighting that misdiagnosis can easily escalate into an act of medical negligence.
Research-proven gender disparities in diagnosis and outcomes
Moreover, a study from the University of Copenhagen reveals that women, on average, receive their first hospital diagnosis at an older age compared to men across all diseases studied [5].
Cardiovascular issues, autoimmune diseases, cancer, neurological disorders, and endometriosis are among the most misdiagnosed conditions in women.

Image of the conditions most misdiagnosed in women
Misdiagnosis survey
1 in 4 women surveyed had a gynaecological or female-specific illness misdiagnosed
Our survey revealed that 24% of women experienced a misdiagnosis of a gynaecological condition, including endometriosis, PCOS, pregnancy, ovarian cysts, and period pain, which highlights a significant problem area in women’s health care. An analysis by Higgs LLP of the 2022-2023 NHS annual report and accounts data found that gynaecology made up 6% of the 10,062 claims made which amounts to over 600 cases. This statistic underscores a broader issue, particularly when compared to the fivefold disparity in research funding for erectile dysfunction (which affects 19% of men) versus premenstrual syndrome, which affects 90% of women [6].
“Just normal women’s problems” or endometriosis
Among the gynaecological conditions listed, endometriosis emerged as the most frequently misdiagnosed, affecting nearly 1 in 10 women surveyed (7%). A heartbreaking statement from our survey revealed a participant whose debilitating symptoms were dismissed as “just normal women’s problems” by her doctor.
This sentiment is supported by a survey from Endometriosis UK, which found that approximately 74% of women with the condition had to visit five or more doctors before receiving a correct diagnosis, and 47% had seen their doctor ten or more times. Disturbingly, 78% of these women reported that their concerns were minimised, with doctors telling them they were “making a fuss about nothing” [7].
Following endometriosis, the second most misdiagnosed condition in our survey was polycystic ovary syndrome (PCOS), reported in 5% of responses. This is particularly troubling given that PCOS affects 1 in 8 women in the UK [8], highlighting a gap between prevalence and adequate medical recognition.
Additionally, 4% of women aged 16-34 reported that their pregnancies were misdiagnosed, with one participant sharing, “I was pregnant, but the doctor said that I was not pregnant. Due to negligence, I had a miscarriage.”
This troubling reality reflects a broader issue in women’s health care, where less than 2.5% of publicly-funded research is allocated to this critical field.
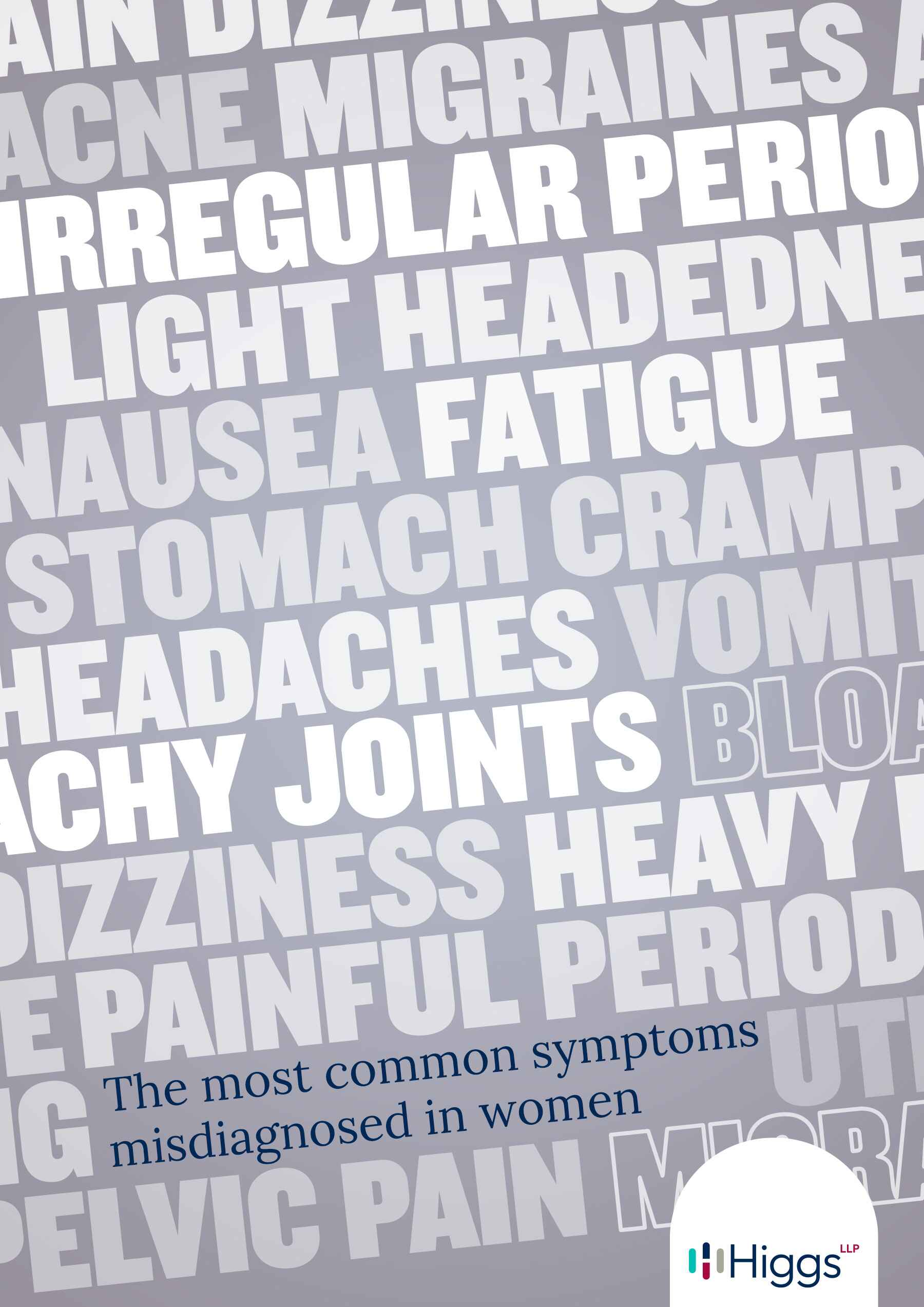
Words of most common symptoms misdiagnosed in women
More than 1 in 20 had mental health conditions or autism misdiagnosed
Our survey revealed that neurological and psychiatric conditions, such as depression, anxiety, eating disorders, ADHD, and autism, are also frequently misdiagnosed in women, with these issues appearing in 6% of the participants we studied. A worrying example from a younger participant illustrates this concern: she was dismissed as “an ordinary teenager” by her doctor, overlooking her genuine struggles.
Research has found that depression may be misdiagnosed in 30-50% of female patients [9] and with 1 in 5 women having a mental health problem such as depression or anxiety [10], the possibility for misdiagnosis grows increasingly concerning. Adding to this complexity, research shows that medical misdiagnoses of physical conditions can induce depressive reactions in female patients [11]. After reading the responses women received from healthcare professionals about their medical issues, this was no surprise. One participant told us that her doctor’s advice for their medical condition was to “put up with it. It’ll pass after you have a family.” Additionally, cases of potential medical gaslighting were reported, such as one woman whose doctor insisted that her symptoms were “all in your head,” telling her there was “nothing” wrong.
Misinterpretation of hormonal disorders in women
Our survey revealed that 1 in 20 women reported experiencing a misdiagnosis related to their hormonal conditions, with thyroid disorders alone being misdiagnosed in 2.4% of participants.
Hyperthyroidism, or an underactive thyroid, is ten times more common in women than it is in men. However, despite this, new research from the University of Aberdeen found that women struggle to get a hypothyroidism diagnosis as their symptoms are too often misdiagnosed as depression or menopause [12].
Our findings underscore this issue, revealing that women’s thyroid problems are often misinterpreted as merely “stress and being over-tired.” This misdiagnosis reflects a broader systemic issue where women’s hormonal health concerns are too readily dismissed or mischaracterised. Our survey participants shared disheartening experiences of being told that their genuine symptoms were simply “normal” for women, rather than being addressed with the medical attention they warranted.
Menopause and perimenopause often go unrecognised
It is estimated that up to 1 in 3 women may face misdiagnoses regarding menopause and its associated symptoms, often requiring between two and five medical appointments before a correct diagnosis is made [13]. In our survey, over 3% of respondents reported that their menopause was initially misdiagnosed, reflecting a troubling pattern.
This issue is expedited by a significant lack of investment in medical research and the stigma surrounding menopause which has led to too many doctors prescribing antidepressants instead of HRT because they lack sufficient training and information [14]. The gap in research funding and attention means that many women continue to face prolonged periods of uncertainty and inadequate care for what should be a well-understood aspect of their health.
The most commonly misdiagnosed symptoms
Women often present with a wide array of symptoms that are frequently misdiagnosed, leading to prolonged suffering and delayed treatment. The top ten most common misdiagnosed symptoms found from our survey were as follows:
- Fatigue (31.40%)
- Lightheadedness and dizziness (25.20%)
- Irregular periods (22.80%)
- Painful periods (22.60%)
- Heavy periods (20.80%)
- Stomach cramps (19.80%)
- Achy joints (18.20%)
- Headache (17.20%)
- Migraines (16.60%)
- Nausea/vomiting (15.60%)
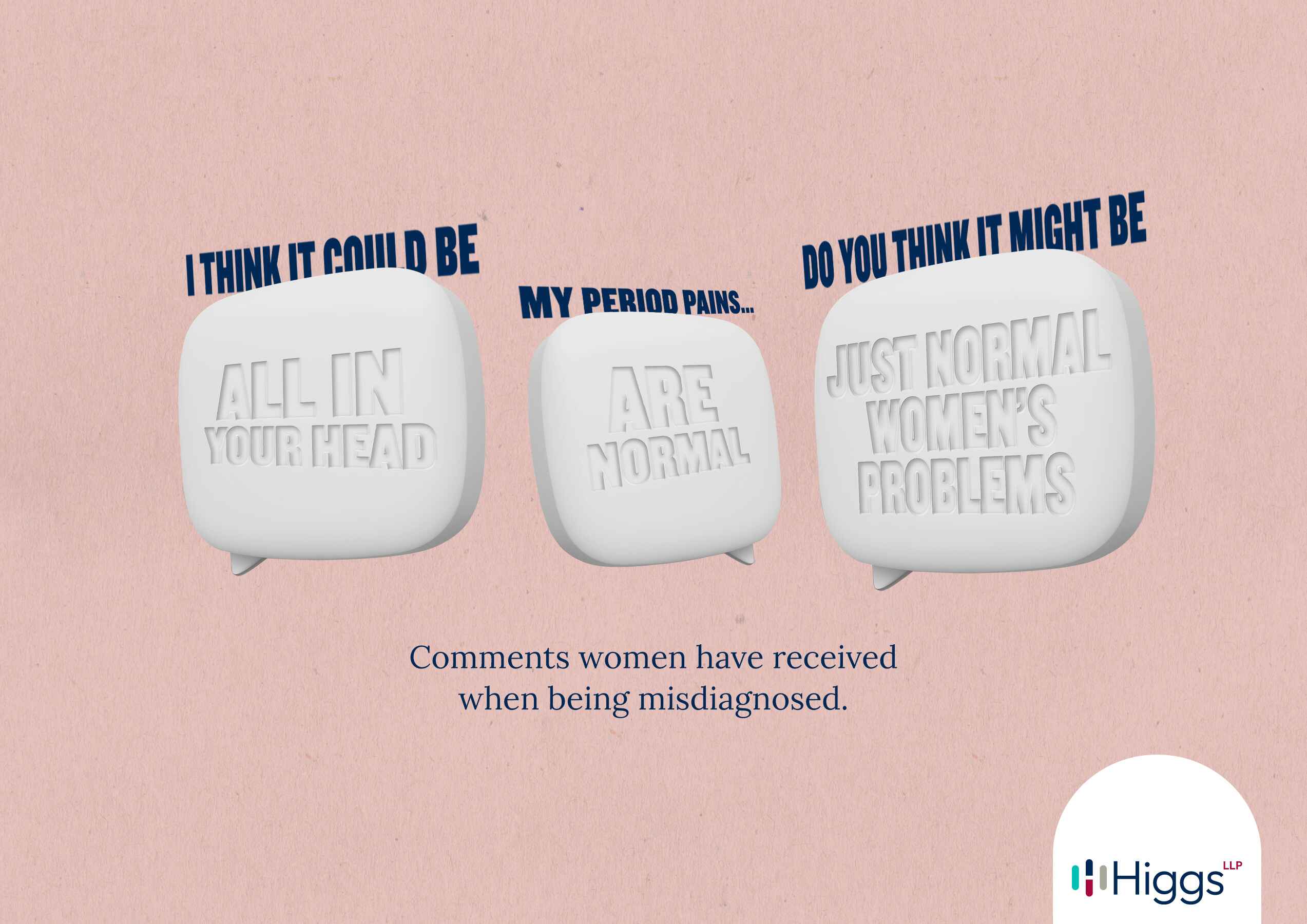
Comments women received when being misdiagnosed
Less common misdiagnosed symptoms included the following:
Less common misdiagnosed participant symptoms
Symptom |
% of participants |
|
Pelvic pain |
13.80% |
|
Bloating |
13.40% |
|
Sweating and hot flashes |
12.80% |
|
Acne |
11% |
|
Urinary tract infections |
9.20% |
|
Pain during sex |
9.20% |
|
Infertility |
8.60% |
|
Diarrhoea |
7.60% |
|
Constipation |
7.40% |
|
Heartburn or indigestion |
6.60% |
Despite women constituting 51% of the population, there remains a significant gap in research and data on how medical symptoms impact women differently from men [15]. This disparity may explain why, of the 500 women surveyed, Higgs LLP documented over 90 symptoms inadequately diagnosed by healthcare professionals.
Illnesses given as wrong diagnoses
Women often receive dismissive attitudes toward their symptoms, and our survey responses highlighted this troubling trend. Women shared disheartening experiences, such as, “I was told that this was normal for a woman in her 30s” or “I was told it was just typical period issues.” These responses from healthcare professionals highlight that women often face widespread dismissive attitudes towards their symptoms, which can lead to serious conditions being overlooked or misdiagnosed.
Our survey revealed that women’s symptoms are frequently misunderstood or minimised, with conditions such as anxiety and depression (4.6%), irritable bowel syndrome (4%), stress (3.6%), period problems (2.8%), and skin conditions (2%) often being mistakenly identified as the root cause of their issues.
It could be argued that poor interpretations of symptoms are a consequence of GP waiting times and the pressure put on healthcare professionals. NHS data reveals that 1 in 20 patients has to wait at least four weeks to see a GP. Furthermore, 5.4 million patients (17.3%) were forced to wait at least two weeks after booking to see a GP, practice nurse, or other health professional [16].

Most commonly prescribed medication on misdiagnosis
This could be one of many reasons why our survey found that it took the majority of women 3-6 months to gain the right diagnosis. Alarmingly, 20% of participants reported that it took them over two years to finally receive a proper diagnosis and effective treatment. Despite understanding the pressures faced by the NHS, we’d like to echo that this is no excuse for women to face a lack in standard of care or in more serious cases NHS negligence.
Inappropriate treatments prior to correct diagnosis
Our survey revealed that a significant number of women received inappropriate treatments before finally obtaining a correct diagnosis. Specifically, 1 in 4 women reported being wrongfully prescribed pain medication in an attempt to manage their symptoms without addressing the underlying cause. This is particularly concerning as research indicates that there is an opiate gender gap in which women in England are nearly twice as likely to be prescribed powerful opiate painkillers compared to men [17]. This highlights a troubling trend where female pain may be overmedicated rather than thoroughly investigated, which may have contributed to the doubling of opioid-related deaths over the past decade [18].
Following closely behind, 1 in 5 women found themselves prescribed antidepressants or SSRIs as doctors overlooked the root cause of their condition. This aligns closely with research regarding stereotypes of the “hysterical woman” whose physical concerns are addressed as psychological causes rather than somatic pain [19]. This links to further research that rates of prescribing antidepressants were higher for women (1.5 times those of men) [20]. In addition to these treatments, 16% of women reported being prescribed contraceptive pills to manage their symptoms, a trend that reflects a broader concern about the overprescription of hormonal contraceptives.
Between 2022 and 2023, 4 million people were prescribed the mini-pill and 3 million the combined pill [21], with many prescriptions serving purposes beyond contraception, such as acne treatment or alleviating period cramps. However, this practice can mask more serious underlying conditions. As one participant shared with Higgs LLP, she was told that her symptoms were merely due to her young age and “bad periods,” a dismissive attitude that led to years of unnecessary suffering before she received an accurate diagnosis.
In addition to pain medication, antidepressants, and contraceptives, other commonly misprescribed treatments included anti-inflammatory medication (11.6%), hormone replacement therapy (5.6%), laxatives (5%), oestrogen (4.4%), progesterone (3.2%), and topical creams and lotions (2.4%). These instances of wrongful prescribing not only delayed appropriate care but also perpetuated unnecessary discomfort and frustration for many women.
The link between misdiagnosis and medical negligence
When a doctor or healthcare professional misdiagnoses someone, it can not only be a medical error but also a case of medical negligence. Healthcare professionals are entrusted with a fundamental duty of care, tasked with ensuring patient safety and providing accurate diagnoses. When this duty is breached through misdiagnosis, patients may receive inappropriate treatments that fail to address the underlying causes of their symptoms or no treatment at all. Such failures can lead to the progression of serious conditions and expose patients to unnecessary and painful side effects from incorrect medication.
Clare Langford, Medical Negligence expert, comments:
“Misdiagnosis becomes a legal matter of medical negligence when it stems from a failure to adhere to established diagnostic standards or from inadequate follow-up procedures. This can include neglecting to consider alternative diagnoses, failing to thoroughly assess a patient's medical history, or making errors in documentation. For instance, if a healthcare provider dismisses a patient's symptoms as trivial without performing essential diagnostic tests, and the patient is later found to have a severe condition like cancer, this situation exemplifies both misdiagnosis and a failure in patient care, potentially qualifying for a medical negligence claim.”
Methodology
A 500-person survey was conducted, asking female participants a screening question of ‘Have you ever been misdiagnosed by a medical professional?’ followed by 5 questions on their misdiagnosis. The results were then analysed.
Sources
- Nature Communications: Population-wide analysis of differences in disease progression patterns in men and women
- Northwell Health: Gaslighting in women’s health: No, it’s not just in your head
- Ibid.
- Ibid.
- Nature Communications: Population-wide analysis of differences in disease progression patterns in men and women
- ResearchGate: Why do we still not know what causes PMS?
- Endometriosis UK: “Dismissed, ignored and belittled” The long road to endometriosis diagnosis in the UK
- Verity: PCOS
- PubMed: Problems in accurate medical diagnosis of depression in female patients
- NHS: Adult Psychiatric Morbidity Survey: Survey of Mental Health and Wellbeing, England, 2014.
- PubMed: Problems in accurate medical diagnosis of depression in female patients
- Women’s Health: Women with underactive thyroids are being told they are menopausal or depressed
- Kindra: Nearly 1 in 3 Women Have Had Their Menopause Symptoms Misdiagnosed
- Fawcett: Menopausal Women Let Down By Employers And Healthcare Providers
- GOV.UK: Government launches call for evidence to improve health and wellbeing of women in England
- The Guardian: One in 20 patients in England wait at least four weeks to see GP, figures show
- The Guardian: Women in England almost twice as likely as men to be prescribed opiate painkillers
- Ibid.
- National Library of Medicine: “Brave Men” and “Emotional Women”: A Theory-Guided Literature Review on Gender Bias in Health Care and Gendered Norms towards Patients with Chronic Pain
- GOV.UK: Prescribed medicines review: summary
- The Guardian: Contraceptive pill to be available on high street without need for GP visit
This information is for guidance purposes only and does not constitute legal advice. We recommend you seek legal advice before acting on any information given.

